It is rarely possible to diagnose thoracic osteochondrosis of the spine (GO), in contrast to the cervical and lumbar, which are found in every 2-3 patients aged 18 and over. This phenomenon is explained by the special structure of the thoracic part - the presence of a larger number of discs, which in turn have a finer structure. This part of the spine has low mobility, and accordingly, the load on it is not high, since the main "blow" is taken by the sternum together with the ribs.
The main reason why the development of chest pathology begins is an increase in the load on the intervertebral discs and, as a result, a violation of metabolic processes, as well as their structure. . . In the presence of such an ailment, the shock-absorbing properties of the disc are lost, the fibrous ring becomes thinner, dries up, after this process, the nerve endings become inflamed, the person feels constant pain, discomfort, and motor activity decreases. With the rapid course of the disease, it affects the ligaments of the spine and articular joints.
Now, many experts have taken it as a rule to classify osteochondrosis not by the stages of the course, but by degrees, which are additionally distinguished by the peculiarities of the symptomatology.
If we take into account the general symptomatology, then osteochondrosis of the thoracic region is not so pronounced, unlike its other types, nevertheless, there is a characteristic clinical picture. So, the patient may complain about the presence of the following signs:
- pain in the thoracic region, often aggravated by prolonged exposure to one position or at night;
- painful sensation between the shoulder blades, while, it increases with raising the arm or after physical exertion;
- discomfort, pain when trying to breathe deeply, this symptom is also noted when you exhale;
- while walking, there is soreness in the ribs and a feeling of squeezing in the chest area.
Such manifestations can accompany a person for several weeks, which should be regarded as an exacerbation of the disease.
What other symptoms can be observed with HO? In addition to the main clinical picture, in some cases the following manifestations are possible:
- numbness of the upper extremities, a feeling of "goosebumps" running through the skin;
- disruption of the organs of the gastrointestinal tract;
- feeling of cold in the legs, the inability to warm them.
Also, the characteristic signs of such an ailment are dorsago - the occurrence of sharp pain between the shoulder blades and dorsalgia - a slow pain syndrome that does not have a pronounced picture.
It should be noted that, like any other type of osteochondrosis, chest disease often affects people leading an inactive lifestyle. Constant sitting at the computer, stoop, heavy physical exertion, also become a provoking factor in the development of the disease.
How does the disease manifest in women and men
The development of degenerative-dystrophic processes in the thoracic region in patients is considered as a diagnosis - thoracic osteochondrosis. With this disease, there is the destruction of the intervertebral discs and malnutrition in the structures of the connective tissue. In addition, the blood circulation process is disrupted, since the chest area is inactive. And the pain syndrome itself occurs due to pinching of nerve endings during the progression of pathology.
As the statistical data indicate, HO is diagnosed in women at times more often than in men, and at the same time at a younger age. The main reason for this phenomenon is the change in hormonal levels when entering the menopause phase. The impetus for the development of the disease is also osteoporosis, which is often detected in women during the onset of menopause.
Therapeutic measures are developed taking into account the clinical picture of pathology. Severe symptoms do not appear immediately, it often takes a long time to suspect the presence of the disease. Specifically, it is possible to establish a diagnosis already in the course of a pronounced picture, when the symptoms have become obvious. When it comes to a pronounced period, then two types of symptoms should be distinguished here:
- Development of painful sensations. . . Here we are talking about the occurrence of pain in the thoracic region, between the shoulder blades, radiating to the area of the solar plexus. Pain syndrome can migrate to the neck area, mimicking cervical osteochondrosis and into the arm. Often women observe pain in the mammary glands, confusing them with breast pathologies. As a rule, pain sensations are not permanent, they are aching, but at the same time, they do not have intensity.
- Blood pressure disorder. . . With breast osteochondrosis in women, there is such a thing as hypertensive syndrome, which is characterized by increased pressure and can provoke a hypertensive crisis. A distinctive feature of normal hypertension may be the presence of a minimal effect from the use of drugs that lower blood pressure. In the case when you have had similar situations, you should additionally consult with a vertebrologist.
In addition to the above, other signs of degenerative-dystrophic disorders in the thoracic spine should be distinguished:
- Pain on the left side of the thoracic region,not associated with heart damage. . . In medical terminology, this phenomenon is called cardialgia. It is not difficult to diagnose it, since with the development of such a symptom, it cannot be stopped by the use of cardiac drugs.
- Disruption of the functioning of the digestive system. . . Often, with the onset of the progression of osteochondrosis, problems begin with the internal organs, more often with the gastrointestinal tract. The most striking example is the formation of heartburn, an increase in acidity and a feeling of constant bloating (flatulence). Among other things, there may be problems with the digestion of food - nausea after eating, heaviness, bloating. Against the background of all of the above, the work of the chair is also disrupted - frequent constipation or diarrhea.
- Respiratory disorders. . . Since the dystrophic process takes place in the chest area, cases of a violation of the respiratory system are not uncommon. All this is accompanied by unreasonable dizziness, general weakness, shortness of breath and other signs that may indirectly resemble heart pathology or problems with pressure (arterial / intracranial).
With regard to therapy, it largely depends on the signs of the pathological process. To relieve pain, pain relievers are prescribed, including NSAIDs in the form of ointments or gels. During the period of exacerbation, muscle relaxants are more effective, they reduce spasm of smooth muscles, relax muscles, relieve pain syndrome, reviews of their use are positive. When the pain becomes completely unbearable, blockade with pain relievers is used.
Thoracic treatment
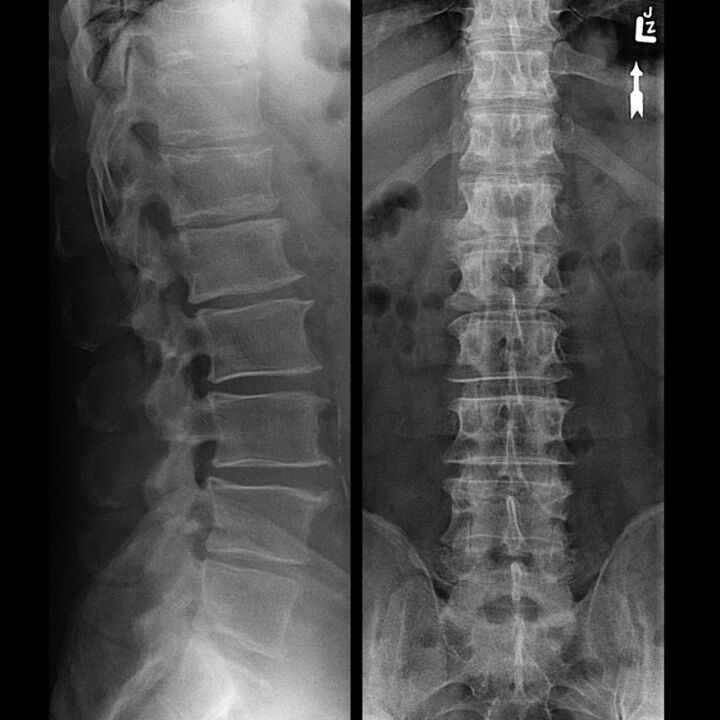
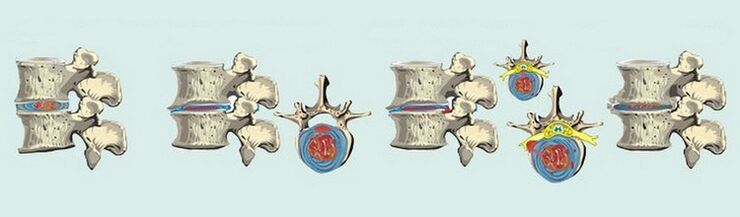
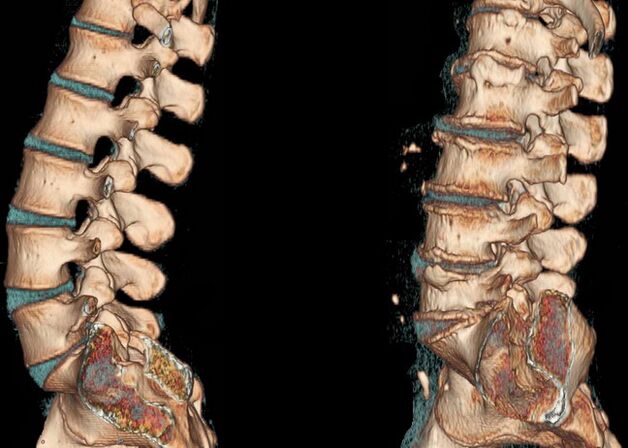
How exactly GO will manifest itself depends on the pathological changes that take place in the intervertebral discs. It is customary to distinguish four stages of the course of degenerative-dystrophic disorders in the chest:
- The first. . . Symptoms are not particularly pronounced, however, the process of dehydration of the disks of the thoracic spine has already started. As a result, they lose their elasticity, begin to acquire a more flattened appearance, but, at the same time, they can still withstand certain loads. Occasionally, painful sensations of the aching type are disturbed, but not mild and often do not require taking painkillers.
- The second. . . At this stage, negative changes affected the annulus fibrosus, various types of damage are observed - cracks, loss of stability. There are changes in the pain syndrome, it becomes more intrusive, palpable, intensifies with an increase in motor activity - bends, turns.
- The third. . . On x-rays, the rupture of the annulus fibrosus is clearly visible, and a hernia begins to form. Pain sensations become clearer, from a whining character can flow into a sharper one, intensify with movements and even at rest.
- Fourth. . . Spondyloarthrosis is actively developing, against the background of convergence of the vertebrae and erasure of discs. As a result, the connective tissue of the annulus fibrosus is replaced by bone tissue, which significantly limits motor ability.
The clinical picture of thoracic osteochondrosis is such that it is more likely to diagnose this disorder:
- Pain. . . Almost always, its localization is in one specific place, often on the left. After some time, it spreads throughout the entire chest area, breathing becomes difficult, it becomes difficult to climb stairs or exercise.
- Increased pain. . . Strengthening occurs when turning or tilting, in general, with any physical activity, the same is observed when trying to take a deep breath.
- Muscle spasm. . . Muscle spasm is added to the above symptoms, the contraction falls mostly on the upper back. In more rare cases, such a symptom is present in the lumbar region.
Separately, it is worth noting intercostal neuralgia, which tends to last for several weeks and then disappear on its own. During this time, a person is accompanied by chest discomfort, aggravated by movements, discomfort when trying to take a deep breath in / out. Women may get the impression of having problems with the mammary glands, which will make them think about treating them, and in men, a feeling of a foreign object behind the breastbone.
It should also be noted that the entire clinical picture described above intensifies at night or after hypothermia. The next morning, as a rule, it becomes easier, but towards evening everything repeats again.
How to treat, what methods exist, what to take? With regard to therapeutic measures, they should be started as early as possible. Often, at the very first stages, it is possible to do without even the use of medications, but only with regular gymnastics — exercise therapy.
Later stages of the development of pathology, at 2 degrees, involve the use of drugs. This includes various groups of drugs, the most popular are presented in the table below.
| Group of medicines | The main action of the medication |
|---|---|
| Pain relievers, analgesics | They relieve pain syndrome, reduce its manifestation. |
| Non-steroidal anti-inflammatory (NSAID) | Eliminate inflammation, relieve pain, swelling. |
| Chondroprotectors | They increase the production of intra-articular secretions, slow down the process of cartilage destruction, and reduce the manifestation of the inflammatory process. |
| Muscle relaxants | They reduce the tone of skeletal muscles, have a relaxing effect, and help to effectively cope with back pain. |
| Sedatives, sedatives | For more effective therapy, since severe pain can provoke stress, which worsens the effect of treatment. |
In addition to essential medicines, a course of medicines-vitamins is recommended.
In the case when the entire clinical picture is aggravated, the main goal of therapy will be to relieve symptoms. For a more pronounced and quick action, analgesic drugs are prescribed in the form of injections, as well as of the steroid type.
After eliminating the exacerbation and achieving stability of the state, it is necessary to start basic therapy. A fairly wide range of drugs can be prescribed, since only a complex effect on the disease can give positive results.
The main medicines are described in the table above, then in more detail about them. So, the basic treatment will include the appointment of such medications:
- Chondroprotectors.They are used in tablet form and for local therapy, in the form of ointments or gels. It is impossible to exclude the use of such drugs, they are the basis for complete therapy. Their action is aimed at inhibiting the process of destruction of cartilaginous tissue and further progression of dystrophic changes. In addition, they increase the regenerative capacity of the cartilage. However, it is impossible to completely get rid of the pathology with the help of such a medicine; it should not be regarded as a panacea.
- Vasodilator. . . They are necessary to improve blood circulation and, accordingly, nutrition in the affected area. Most often, a fairly effective drug is prescribed that improves blood microcirculation, helps to cope with pain that occurs at rest.
- Local therapy. . . For the best effect, ointments or gels are prescribed. So, good results can be achieved only with the help of a complex effect, therefore, when prescribing NSAIDs and chondroprotectors, it is customary to additionally recommend ointments of the same pharmacological groups. Also popular are creams based on bee or snake venom, they have a pronounced analgesic effect and are a good addition to the main therapy.
- Vitamins. . . In particular, vitamins of group B are prescribed. They have analgesic properties, help to cope with inflammatory processes and with infringement of nerve endings.
- Without fail, along with the drug effect, a course of physiotherapy, therapeutic massage, exercise therapy is prescribed.
What other methods of therapy should be included in the treatment of chest osteochondrosis? An experienced professional will strongly recommend the following techniques:
- magnetotherapy, electrophoresis, therapeutic mud;
- complex of physiotherapy exercises;
- acupuncture, acupressure.
It is also recommended to adhere to a certain diet, you should exclude the use of alcohol, spicy foods, reduce the use of salt.
Particular attention should be paid to therapeutic exercises, it should be carried out daily, and preferably several times a day. Please note that the set of exercises is developed individually by the attending physician - an orthopedist or traumatologist. Physical education is performed in the absence of exacerbation, when there is no pronounced pain, in case of acute pain syndrome, maximum rest must be adhered to.
Sports with osteochondrosis is not the last thing. With this pathology, it is important to regularly perform all the prescribed exercises that will strengthen the muscles and positively affect the outcome of treatment.
We should also mention traditional medicine. On the Internet, you can find many recipes based on natural raw materials. It is not recommended to get carried away with folk remedies as an independent method, due to the fact that the effectiveness of them will be minimal, and in many cases zero. However, as an adjunct to mainstream therapy, folk remedies may be recommended. The following homemade recipes are known:
- Ingredients for the first: 3 tablespoons of rye flour, 1 tablespoon of turpentine and a teaspoon of iodine and garlic. Mix everything thoroughly and use as an ointment at night.
- For the second: 5 tablets of metamizole sodium and 5 ml of camphor alcohol. Bring the tablets to the state of a powder, then pour in alcohol and apply overnight in the form of applications.
A needle applicator is considered another alternative therapy. Its action is aimed at reducing pain syndrome through needle massage.

In the case when all the described methods of therapy did not give the desired result or it turned out to be not long-lasting, the question of prescribing an operation is decided. Surgery is necessary when it is not possible to eliminate the pain syndrome, the degenerative-dystrophic process continues to develop, at the same time, there are negative changes in the functioning of internal organs. If the doctor still recommends to you to carry out the operation, then you should not immediately refuse. Timely intervention will allow you to get rid of such a problem, fully restore the work of organs and exclude the further development of complications.
Surgery usually involves two stages. The first is aimed at removing the cause - decompression, due to which the pain syndrome is eliminated. The second stage is the subsequent stabilization of the spine.
Osteochondrosis of the thoracic region is a serious pathology that can not only disrupt the work of the musculoskeletal system, but also negatively affect systems and organs.
It is important to monitor your own health, take preventive measures, monitor your diet, and be smart about physical activity. Regular exercise is an effective prevention of osteochondrosis, but do not forget that any load should be moderate.
Treatment of the cervicothoracic type
Osteochondrosis of the cervicothoracic region is not considered to be an independent pathology. In this case, we are talking about a set of disorders that appear in the intervertebral discs and are capable of affecting muscle tissue, as well as nearby organs.
Cervicothoracic osteochondrosis is far from uncommon, more than 20% of diagnoses are attributed to this ailment. The disease is very insidious, the variety of the clinical picture in many cases makes the doctor suspect about other diseases not related to the spine. For example, a doctor may suggest the presence of angina pectoris, recommend taking a drug, which, in the end, simply will not give any result, and worst of all, it will negatively affect the state of the heart system. For this reason, it is very important to differentiate osteochondrosis from pathologies of internal organs. So, for dystrophic disorders in the cervicothoracic region, the following signs are characteristic:
- frequent headaches;
- loss of strength, followed by dizziness;
- aching pains in the neck, flowing into the shoulders, shoulder blades, a state of muscle stiffness;
- compression of the intercostal nerve roots, hence the pain syndrome, as well as its exacerbation;
- violations of blood pressure, there may be drops from hypertension to hypotension, more often in women;
- decreased visual acuity, problems with the hearing aid (hearing loss);
- in men, a decrease in potency with nervous overload on the background of the disease.
An important point is the formulation of the correct diagnosis; a number of diagnostic measures will be required here, which will include: X-ray examination, ultrasound, MRI, CT.
Comprehensive treatment is mandatory and should include:
- medications;
- various physiotherapy techniques;
- physiotherapy;
- non-traditional therapy (acupressure, acupuncture).
It is also important to take care of non-drug measures, for example: to reduce physical activity, which includes minimizing the load, change the mattress, purchase an orthopedic type pillow.
Atypical symptoms, sensations and pain
In addition to the typical pains that manifest themselves in chest osteochondrosis, there are many atypical pains that cannot be associated with diseases of the spine. However, you should be aware of them:
- Heart pain. . . Often, with such a pathology, pains in the heart appear, while imitating attacks of a heart attack. One distinguishing feature is their duration. Unlike true heart pains, with osteochondrosis, the pain is prolonged, it can bother for several weeks. In addition, the use of traditional medicines does not reduce the manifestation of pain. It is here that it is worth thinking about the presence of another pathology that is not related to the heart.
- Imitationpathologies of the mammary glands. . . This clinical picture applies directly to patients. Often, thoracic osteochondrosis makes one think about breast diseases, since a woman can observe pain in the thoracic region for a long time, spreading to the glands. To identify the true cause of such a symptom, or at least to exclude problems with the mammary glands, is possible only after examination by a mammologist.
- Pain in the abdominal cavity. . . This symptom makes one suspect the presence of gastritis and other diseases of the digestive system. Mistakenly, a gastroenterologist can diagnose pancreatitis or cholecystitis. It is possible to refute or confirm such diagnoses with the help of a thorough examination.
- In addition to these signs, the patient may feel a pronouncedchest discomfortdescribed as having a foreign object. It is often difficult to take a deep breath or exhale, the feeling that it is impossible to breathe in deeply, shortness of breath with little physical activity.
The process of treating degenerative-dystrophic disorders is not easy, it requires a long time, efforts on the part of the patient and qualifications on the part of the attending physician.
Be sure to consult your doctor before treating diseases. This will help to take into account individual tolerance, confirm the diagnosis, make sure that the treatment is correct and exclude negative drug interactions. If you use prescriptions without consulting your doctor, then it is entirely at your own risk. All information is presented for informational purposes only and is not a medical aid. All responsibility for the application lies with you.

























